Understanding Tibial Interlocking Nail Benefits and Risks?
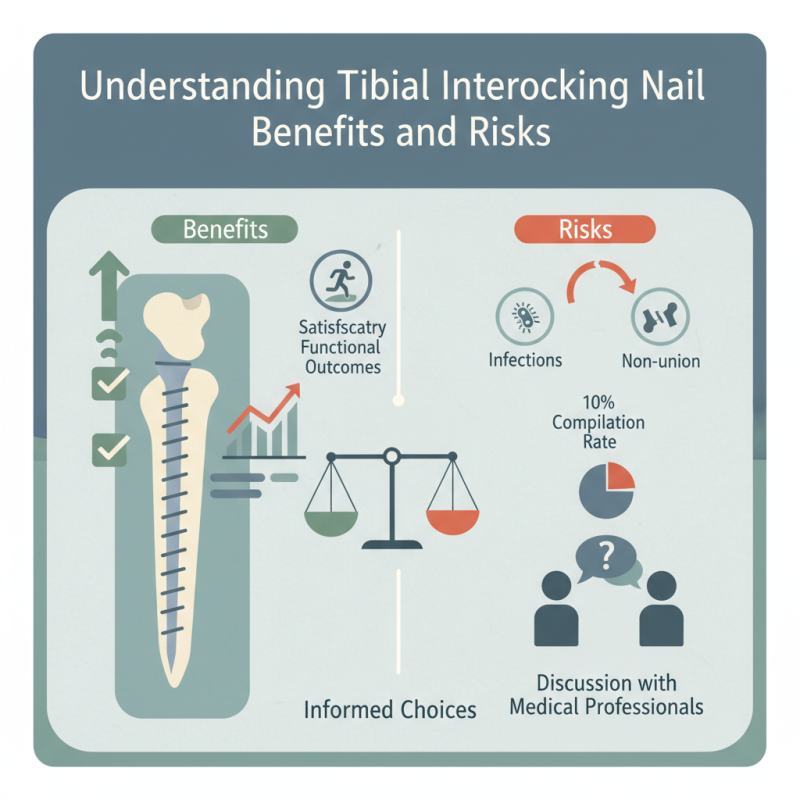
The use of the Tibial Interlocking Nail has gained attention in orthopedic surgery. This technique offers significant advantages for treating tibial fractures. Studies show that the complication rate is around 10% for these procedures, highlighting both their effectiveness and potential risks.
In 2020, data indicated that more than 50,000 patients underwent interlocking nail surgery. Among these patients, 85% reported satisfactory functional outcomes. However, some complications, such as infections or non-union, were observed. It’s crucial to weigh these factors when considering Tibial Interlocking Nail procedures.
Patients deserve informed choices. While the benefits can enhance recovery, the risks demand careful consideration. What works for one individual may not be suitable for another. Therefore, engaging in a thorough discussion with medical professionals is essential.
Overview of Tibial Interlocking Nails in Orthopedic Surgery
Tibial interlocking nails are significant in orthopedic surgery. They provide stability and promote healing in complex fractures. Studies show that these nails can achieve union rates of over 90%. This is a substantial improvement for patients with severe tibial injuries.
The surgical procedure involves inserting the nail through the medullary canal. This method minimizes soft tissue damage. However, complications can arise, such as infection and nonunion. A report from the Journal of Orthopedic Surgery highlighted that about 5% of patients experience these issues, emphasizing the importance of careful patient selection.
Tips: Proper pre-op planning is essential. Surgeons should assess the fracture type, alignment, and patient history. An accurate assessment helps to avoid complications. Maintaining sterile techniques during surgery also reduces infection risk.
Choosing this method must consider all potential risks. Some patients report pain or discomfort at the insertion site. It’s crucial for both patients and surgeons to discuss these outcomes beforehand. Regular follow-up is necessary to monitor healing progress and address any concerns.
Key Benefits of Using Tibial Interlocking Nails for Fracture Repair
Tibial interlocking nails have become a popular option for fracture repair. These nails offer stability and support during the healing process. One key benefit is that they allow for early mobilization. This can help patients regain strength and mobility faster. Additionally, their design minimizes tissue damage. Less damage often leads to quicker recovery times.
However, there are challenges to consider. In some cases, patients may experience complications. Infection can occur, particularly if proper care is not taken. Surgical technique plays a crucial role in preventing such issues. It's essential for surgeons to be well-trained in these procedures. Understanding the patient's condition also affects outcomes.
The use of tibial interlocking nails can be particularly beneficial in specific scenarios. They are effective for complex fractures. These nails can provide better alignment and fixation. However, not every fracture will benefit from this method. Each case should be assessed individually. The trade-offs between risks and benefits demand careful consideration in surgical planning.
Understanding Tibial Interlocking Nail Benefits and Risks
Common Risks and Complications Associated with Tibial Interlocking Nails
Tibial interlocking nails provide essential support for fractured tibias. However, they also carry inherent risks and complications. Studies indicate that complications occur in 10-40% of cases. These can range from minor issues like infection to more severe problems such as malunion or nonunion of the bones.
Infection rates can vary, reported at approximately 5-15%. Surgical site infections pose serious concerns. Patients may experience pain, swelling, or delayed recovery. A deeper issue is the risk of metal fatigue. Implants can weaken over time, leading to a higher failure rate if not monitored closely. This raises questions about the long-term efficacy of tibial nailing.
Another complication is hardware irritation. Patients may feel discomfort where the nail protrudes. This can affect mobility and necessitate further procedures. The psychological impact should not be overlooked. Patients may experience anxiety about recovery or fear of complications. Thus, while tibial interlocking nails serve a vital function, awareness of potential risks is crucial for informed decision-making.
Comparative Analysis: Tibial Interlocking Nails vs. Other Fixation Methods
Tibial interlocking nails have gained popularity in orthopedic practices for their unique advantages. They offer stable fixation for fractures, allowing for early mobility. This is especially important for patients eager to return to normal activities. In contrast, other methods like external fixators might limit movement. Fixators can create discomfort and increase the risk of infection.
However, tibial interlocking nails are not without risks. Potential complications include infection, non-union, or malunion. These issues can lead to prolonged recovery times and additional surgeries. In some cases, the nail may cause irritation to surrounding tissues. Hoisting risks from improperly aligned nails is common, which can complicate healing.
Ten factors need consideration when choosing fixation methods. Surgeons weigh the benefits of stability against potential complications. Personal factors, including age and activity level, also play a crucial role. There is no one-size-fits-all approach in orthopedic treatment. Each case requires careful evaluation and reflection.
Understanding Tibial Interlocking Nail Benefits and Risks
| Feature | Tibial Interlocking Nails | Intramedullary Nails | Plate Fixation | External Fixators |
|---|---|---|---|---|
| Stability | High stability; interlocking prevents rotation | Moderate stability; risk of rotation | High stability with proper alignment | Variable stability; depends on bone quality |
| Nerve Risk | Lower risk of nerve injury | Nerve injury risk during insertion | Nerve injury possible if not carefully placed | Higher risk due to external components |
| Infection Risk | Lower risk due to closed environment | Lower risk as well | Higher risk; exposure during surgery | Moderate to high risk due to external hardware |
| Weight Bearing | Early weight bearing is possible | Weight bearing allowed depending on fracture | Weight bearing generally permitted after healing | Delayed weight bearing recommended |
| Surgical Time | Moderate surgical time required | Shorter surgical time generally | Longer due to exposure and fixation | Variable depending on complexity |
Post-operative Care and Rehabilitation Following Tibial Interlocking Nail Surgery
Post-operative care after tibial interlocking nail surgery is crucial for a successful recovery. Patients often experience pain and swelling. It's essential to keep the surgical area clean and dry. Regular follow-ups with healthcare providers help monitor healing. Patients should follow specific guidelines for physical activity. Weight-bearing restrictions may be recommended initially.
Rehabilitation plays a significant role in regaining strength and mobility. Physical therapy often starts with gentle range-of-motion exercises. Gradually, patients move to strength training for the leg. It's vital to listen to the body. Pain can indicate overexertion. Some may struggle with adherence to the rehabilitation program. Tracking progress can be motivating.
Medication may be prescribed to manage pain and inflammation. Side effects can occur, leading to discomfort. It's important to communicate openly about any concerns. Additionally, emotional support from family and friends can aid in recovery. Engaging in light activities can foster a sense of normalcy. Recovery can feel long and challenging, but persistence is key. Each individual's journey may vary greatly.
